Despite generally favourable research, I've always found the real life application of intermittent fasting is just like any other diet: it comes with potential upsides, and a tonne of potential downsides.
In this short video, I'll cover some of the potential pitfalls, things to avoid, and who best suits an intermittent fasting diet.
Alternatives to intermittent fasting (with most of the benefits, and far fewer downsides)
Having a meal within 60 minutes of waking including protein can have some big benefits long-term.
At My Way Up®, we've helped more than 50 thousand people build better gut health. We've always recommended long-term progress, over short-term "quick fixes."
A simple breakfast incorporating foods such as eggs, quality cheese, collagen, quality milk, and fruit can be used to great effect.
You'll find that your energy is more balanced throughout the day, you retain muscle easier, and your gut function improves.
The downside, is that more regular eating may give you more opportunity to overeat. So as usual, focus on quality of quantity, eat enough to feel energetic, warm, and balanced––and enough that you are making good food choices.
The next step?
Our favourite morning functional foods and supplements are Perfectly Pure™ Collagen, Organic Liver multivitamins, and Opti Flor™ advanced probiotics.
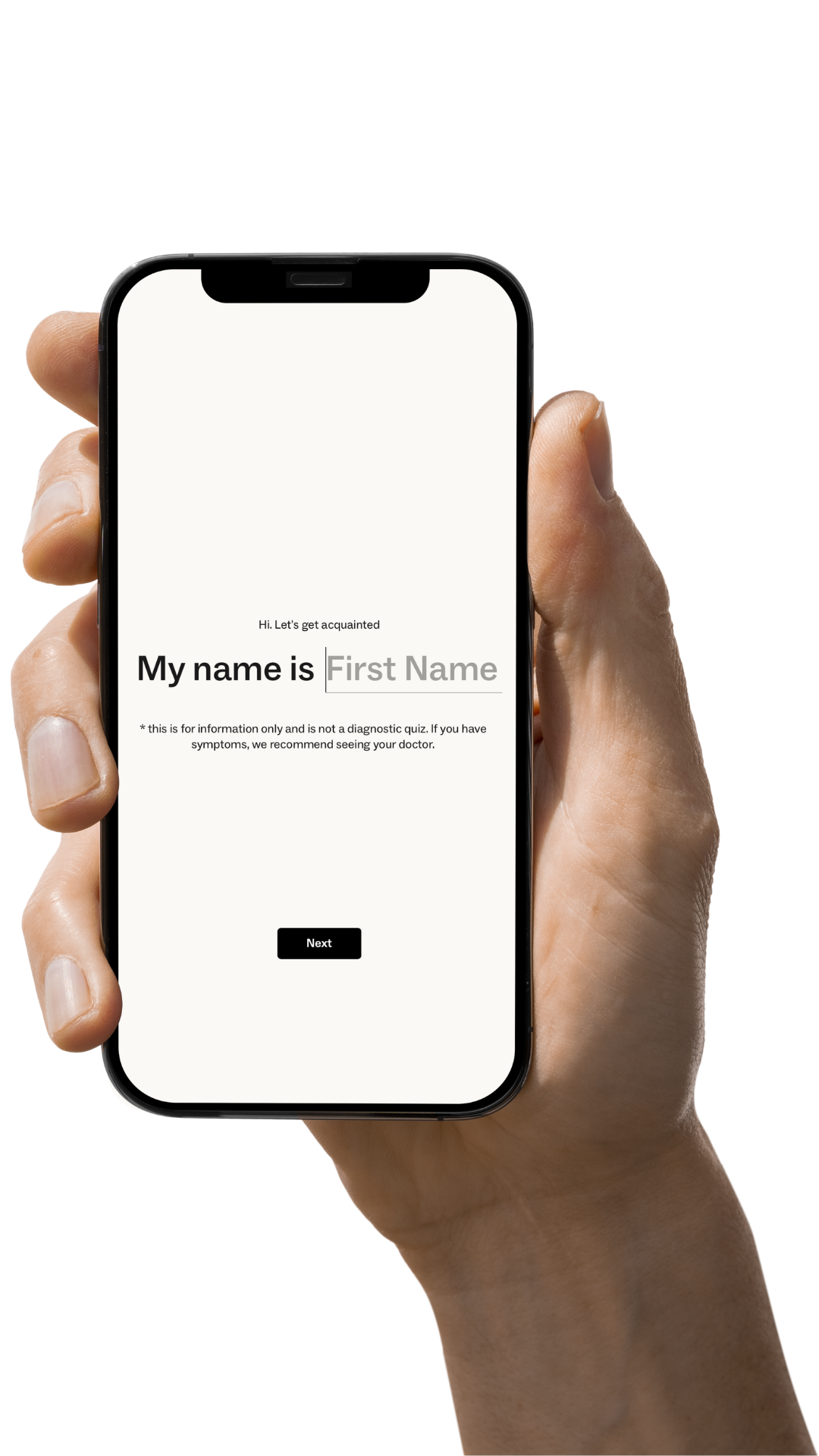
Find out more about our collagen here. Or to find out what products will best help your with your personal symptoms, take our personalised plan builder quiz.